Key learnings
- Discover an overview of the challenges of neuro-oncological surgery and tools for neurosurgeons
- See how Augmented Reality assisted navigation enables more precise brain tumor resection
- Learn about landmarks for navigation and how to achieve optimal registration
Neuro-oncological surgery challenges
In neuro-oncological surgery, the aim is to perform a maximal safe resection and 75% of patients can be treated with a gross total removal, with 25% of patients suffering new neurological deficit. To achieve this aim and determine the best surgical approach, it is critical to identify the lesion and understand the disease evolution as well as know the relevant structures and relationships with the lesion.
All this information can be leveraged within navigation tools to plan the surgery and elaborate case-specific strategies. Several tools also provide assistance during brain tumor surgery, helping to improve the precision of procedures and perform a rigorous quality check.
Tools for neurosurgery & neuro-oncological surgery
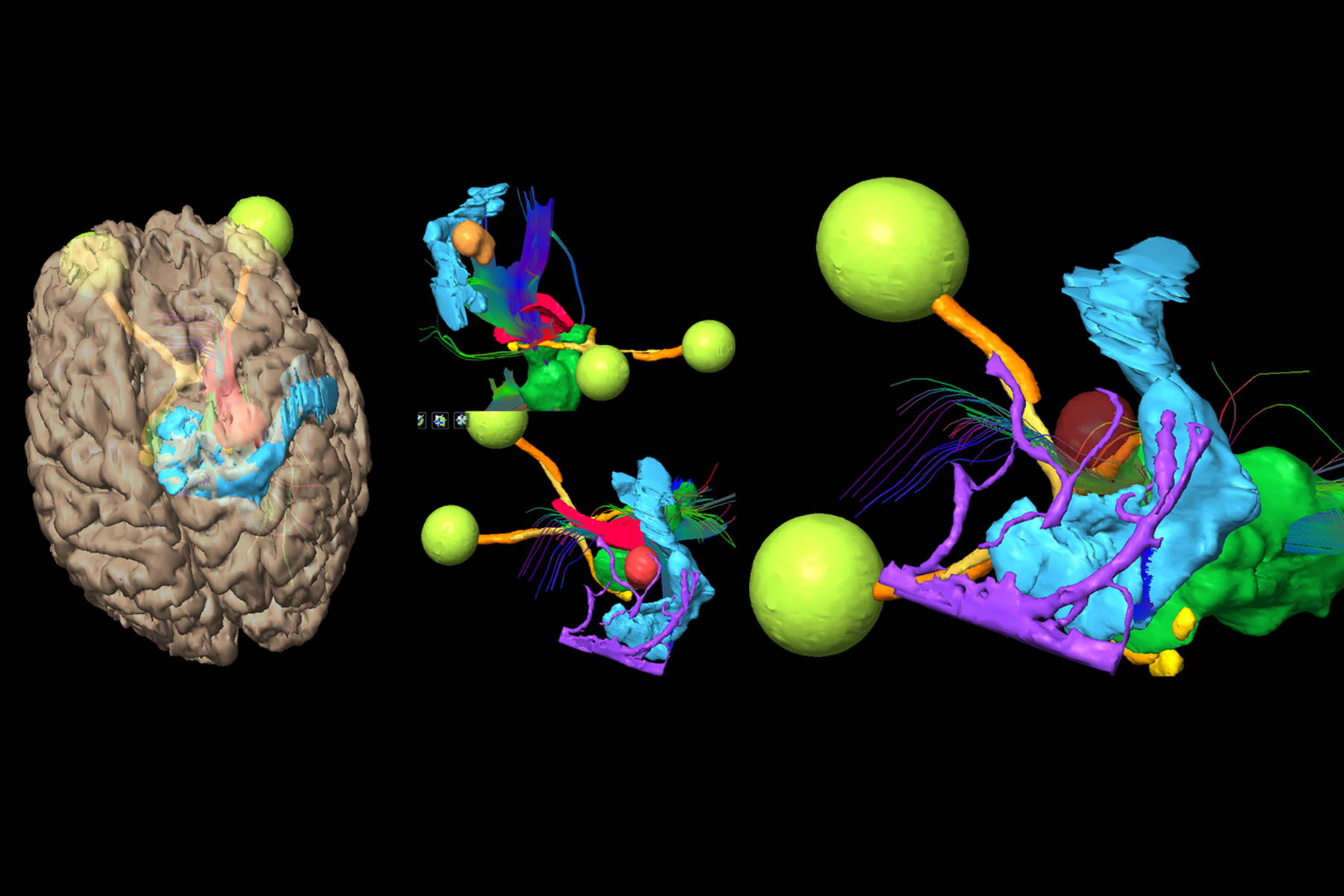
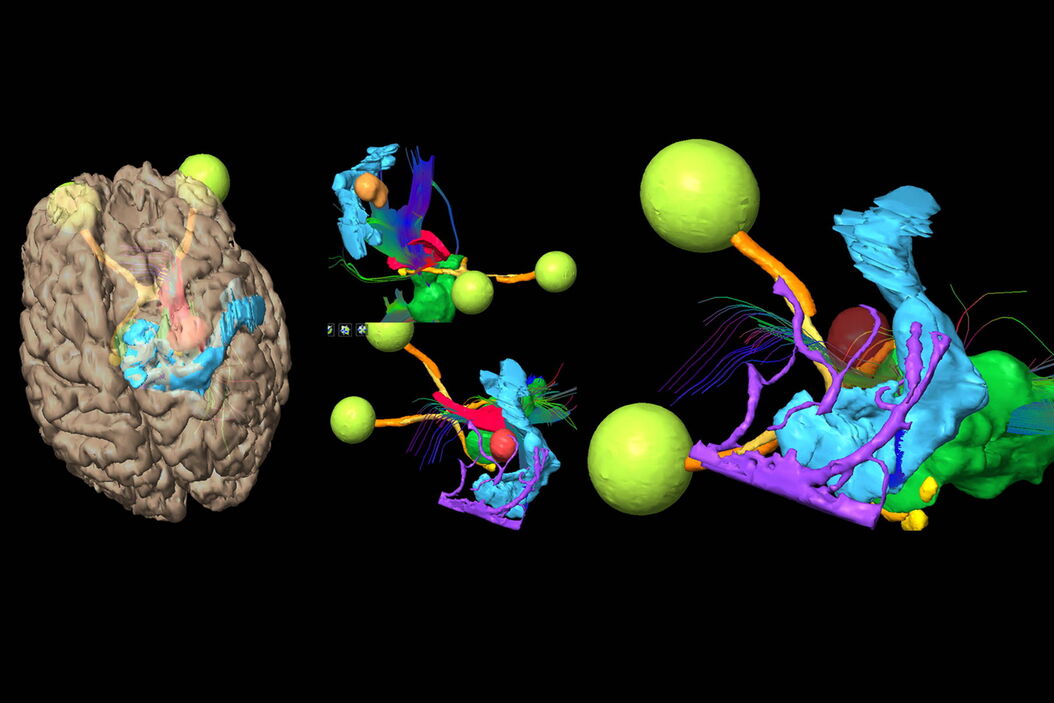
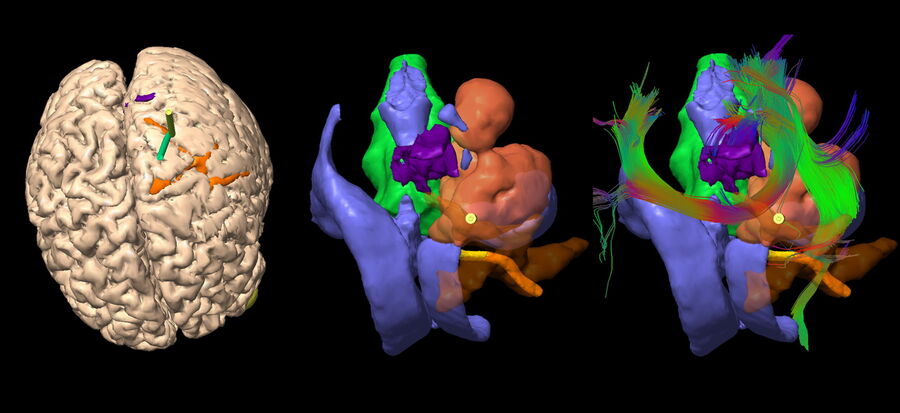
Neurosurgeons have several tools for pre-operative investigations, and in particular imaging techniques: CT-scan, MRI, angiography, ultrasound, transcranial magnetic stimulation, etc. All this information can be integrated through 3D imaging technology, with slices, to obtain one single 3D reference data frame. Then, through segmentation, 3D images can be transposed and become 3D structure objects that can be projected in a 3D environment. It can be through a computer screen display or with new tools, such as a stereoscopic Mixed Reality display.
There is also a wide range of surgical assistance tools. Microscopes provide magnification but also support fluorescence (for example with 5-ALA), neuro-monitoring, neuro-mapping, neuro-navigation and Mixed Reality navigation. The surgeon can access this information in the binoculars, within the operating field.
New hybrid Operating Rooms enable imaging-guided surgery such as angio/hybrid suites with 3D high resolution representation of vessels or intra-operative MRI which allows the repetition of imaging during the operation.
Advanced technologies also include Virtual Reality (immersion in a totally virtual environment), Augmented Reality (addition of information to better interact with reality) and Mixed Reality (addition of virtual objects and interaction with reality).
Enhancing neurosurgery procedures with Augmented Reality navigation
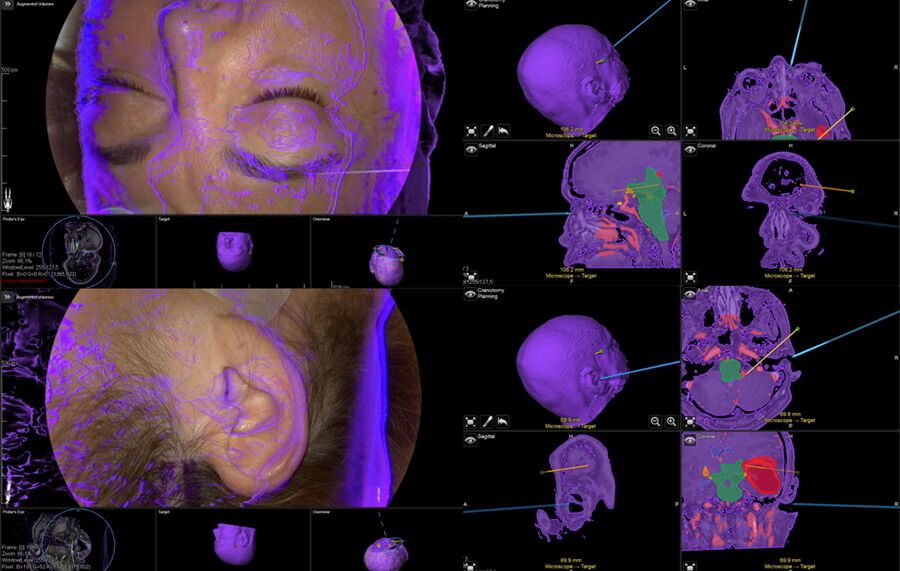
Augmented Reality navigation helps surgeons better plan brain tumor resection surgery, in particular to identify structures at risk and define the optimal surgical trajectory and patient head position. They also support patient and microscope registration. For example, it is possible to perform an accuracy check by verifying the adjustment of the patient skin virtual mask with the patient face.
A study evaluating the precision of operative Augmented Reality compared to standard neuronavigation1 shows that accuracy is 3.5 times higher with Augmented Reality. It also highlights the importance of repeated readjustments to improve accuracy as well as how Augmented Reality increases confidence.
Augmented and Mixed Reality can also support the following steps before and during brain tumor removal: precraniotomy accuracy check using landmarks on the skull, precorticotomy accuracy check and correction, corticotomy and dissection plan, identification of deep structures and accuracy check using the ventricle lumen shape. After removing the brain tumor, it also enables cavity shape conformation inspection.
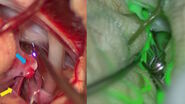
Augmented Reality can be combined with 5-ALA fluorescence switching from one technique to another for greater accuracy, for example when sliding on the tumor edge or inspecting the cavity after tumor removal. A final check with MRI allows to compare pre-operative and post-operative imaging and look for any tumor remnant.
Defining landmarks for navigation
Knowing the signature and target structures is essential to register for different procedures and monitor the precision of the navigation. Signature structures for example include: the lateral sulcus and vein of Labbe for temporal lesions, the callosomarginal and MCA arteries for frontal lesions and the lateral sulcus for parietal lesions.
Based on the landmarks, it is possible to model and simulate the surgery to identify the best patient positioning and design the trajectory. Some surgeries require several trajectories, for example one for the anterior part of the tumor and another for the posterior part.
With Augmented Reality assisted navigation, neurosurgeons know exactly where to look during procedures, enhancing precision and accuracy. By applying these techniques, the Geneva University Hospitals have seen a decrease in the rate of new neurological deficits.
Want to learn more? Register below to watch the full webinar presented by Prof. Philippe Bijlenga and see the clinical cases he shared.
Note: The statements of the healthcare professional in this video reflect only his opinion and personal experience. His statements do not necessarily reflect the opinion of any institution with whom he is affiliated. Please check with your local Leica Microsystems representative for product registration status in your region.