About the Case Study
Key Learnings:
- Learn about posterior segment surgical procedures and their challenges.
- Discover six clinical cases looking at a variety of pathologies including proliferative diabetic retinopathy, retinoblastoma, retinoschisis, retinal detachment, Von Hippel-Lindau (VHL) syndrome and optic disc pit.
- Understand the role of intraoperative OCT, in both rare and more common cases, and how it helps to reveal hidden subsurface details for greater insights and precision in posterior segment surgeries.
Introduction
Prof. Nikolaos Bechrakis uses the Proveo 8 ceiling mounted microscope with the EnFocus intraoperative OCT imaging system, providing enhanced visualization, and helping to reveal hidden subsurface details for greater insights and precision (Figure 1). This configuration also saves space in the operating room.
Clinical Case 1: Proliferative Diabetic Retinopathy
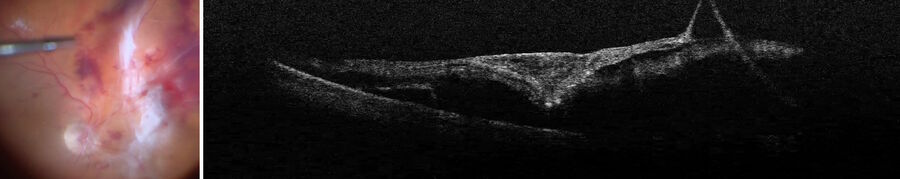
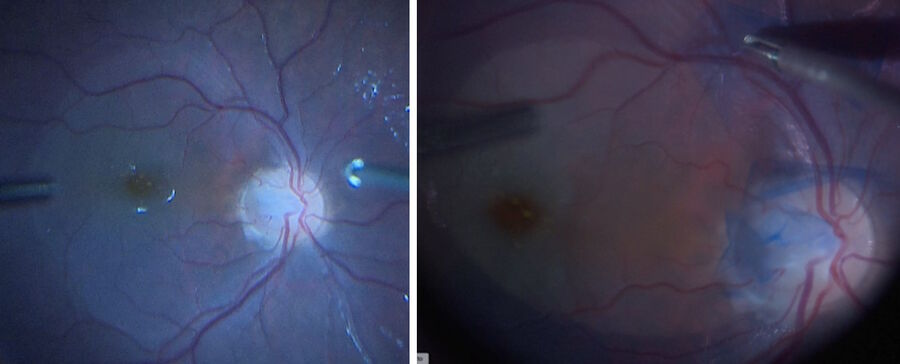
Proliferative diabetic retinopathy is one of the main areas of application of optical coherence tomography, including pre-operatively. The technology supports the visualization of the exact area of scaffolding of the membrane, even when using dye. Allowing the surgeon to see the gaps to grasp the membrane with forceps, without causing damage to the retina just beneath it (Figure 2).
In this case, after peeling the membrane, and with air installation in the eye, there was a reflex of the air bubble (Figure 3). With intraoperative OCT, it was possible to visualize the retina in an airfield situation. This possibility enabled to see how much fluid was under the retina and check for any remaining membrane.
Clinical Case 2: Retinoblastoma
The Essen University Hospital in Germany is the national referral center for retinoblastomas and uveal melanomas.
In this difficult case, the child had a previous retinoblastoma which was treated several years before (Figure 4). The question was whether there was a recurrence of the tumor in the fovea or if it was something else.
The child was put under general anesthesia to perform a comprehensive exam. The intraoperative OCT was used to visualize the white lobule, which could not be done in the clinic. The imaging showed it was subretinal and adherent to the retinal pigment epithelium (Figure 5). This showed it was not a retinal tumor. It was producing retinal atrophy and going up until the internal limiting membrane.
The surgeon concluded it was a fibrovascular scar, a fibrotic choroidal neovascularization (CNV), and not a recurrence of the tumor.
Clinical Case 3: Retinoschisis
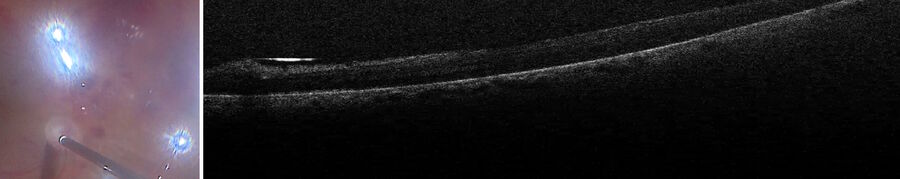
In this case, a child needed to have general anesthesia to examine the eyes. The OCT was especially helpful to confirm the retinoschisis diagnosis.
The Müller cells columns and the exterior part of the retina showed it was not a retinal detachment (Figure 6). There was doubt on whether it could be a very shallow retinal detachment or retinal oedema. The images showed without a doubt it was retinoschisis.
Clinical Case 4: Retinal Detachment
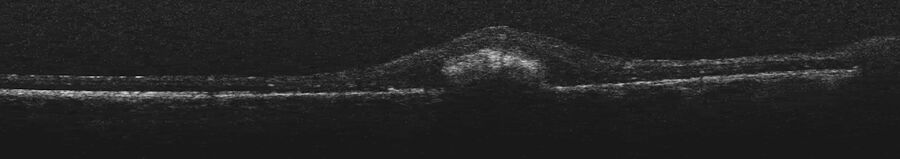
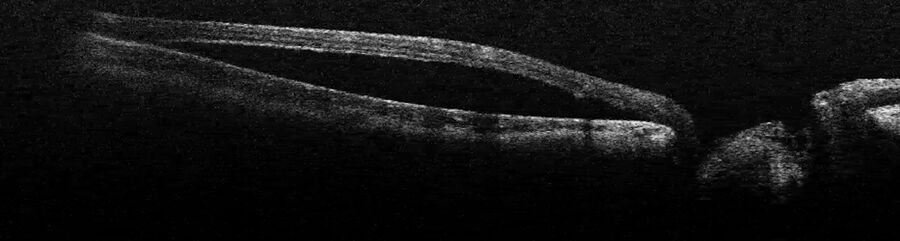
In this retinal detachment case, the fovea and the macula were off. The intraoperative OCT helped to assess the extent of the retinal detachment thanks to the mirroring of the retina (Figure 7). As such, the retinal detachment could be documented within the operating room.
The intraoperative OCT also allowed Prof. Bechrakis to visualize the peripheral problems. Looking for the tears on the retina, the surgeon noticed a peculiar morphology. After indenting the eye with an instrument, the image showed the retina was not only torn, but that there was senile retinoschisis (Figure 8).
Clinical Case 5: Von Hippel-Lindau (VHL) Syndrome
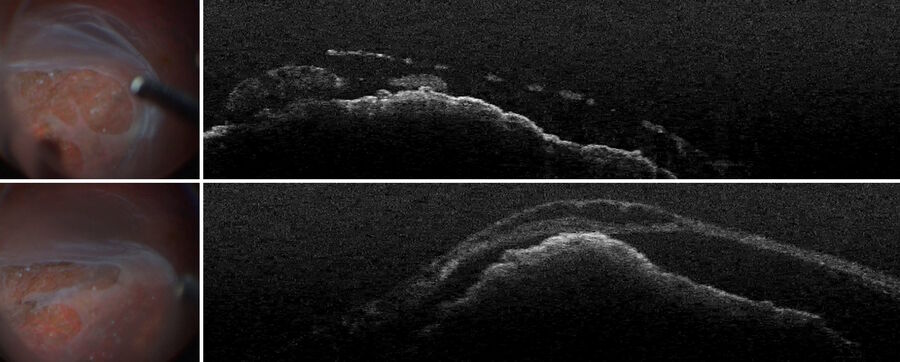
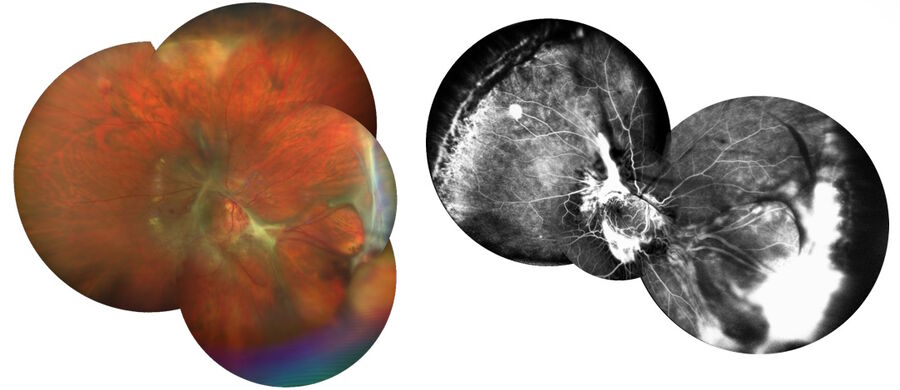
A 30-year-old woman with Von Hippel-Lindau (VHL) syndrome had lost her left eye and her right eye still had relatively good visual acuity, but it was dropping. There were massive membranes that needed to be removed and several hemangioblastomas, including one very large one (Figure 9).
The intraoperative OCT showed the retina was detached and, what was not seen pre-operatively, there was a subretinal membrane and an angioma in the subretinal space (Figure 10). This was extremely useful to understand the exact situation and how the traction retinal detachment was created. The assessment allowed the surgeon to conclude that it was not only created by epiretinal membranes, but also by subretinal membranes.
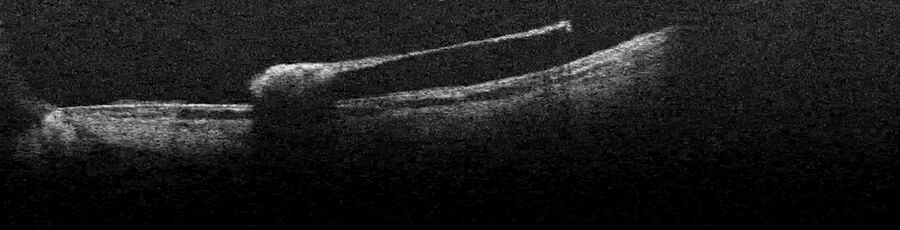
To remove the membranes, a retinotomy was performed and the retina was flipped over (Figure 11). After removal, a control OCT scan was done, and the retina was put back in its position and attached with heavy fluid (Figure 12). At the end of the operation, silicone oil was used.
Clinical Case 6: Optic Disc Pit
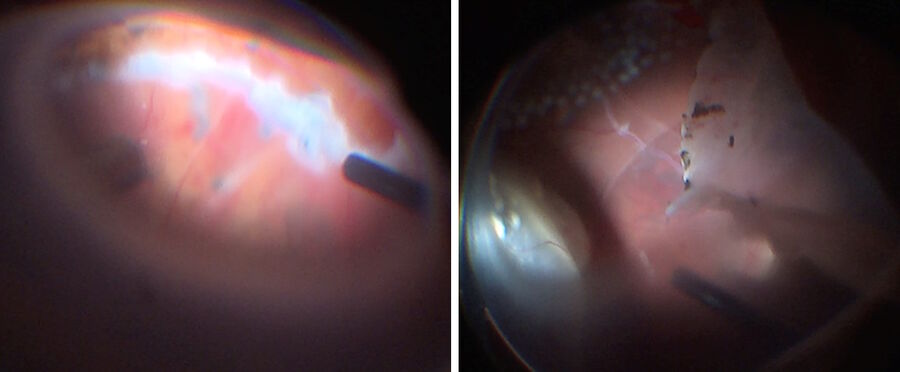
A young girl presented with an optic disc pit. The intraoperative OCT showed the extrusion of the retina next to the optic disc and that the fovea was detached (Figure 13). To treat the patient, vitreous surgery was performed. The vitreous was detached, slightly lifting the retina. Intraoperative OCT provided control throughout the maneuver to avoid too much stress (Figure 14).
The plan for this operation was to produce an internal limiting membrane (ILM) peeling. The ILM was peeled with a 25g instrument after administering ILM dye (Figure 15). After using a modified inverted ILM-flap technique for macular hole, the area where the fluid came into and underneath the retina was sealed. Intraoperative OCT allowed to confirm the ILM was in the adequate position. After the operation, the fluid accumulation slowly decreased and visual acuity improved.
Conclusions
Intraoperative OCT is a valuable tool for posterior segment surgeons. It can improve surgical results and increase the safety of procedures. By using the technology in their practice, surgeons can uncover the situations in which it provides useful information and insights.
Disclaimer: Please note that off-label uses of products may be discussed. Consult with regulatory affairs for cleared indications for use in your region. The statements of the healthcare professionals included in this presentation reflect only their opinion and personal experience. They do not necessarily reflect the opinion of any institution with whom they are affiliated or Leica Microsystems.