Glaucoma surgery clinical case 1: Needling of post-trabeculectomy encapsulated bleb
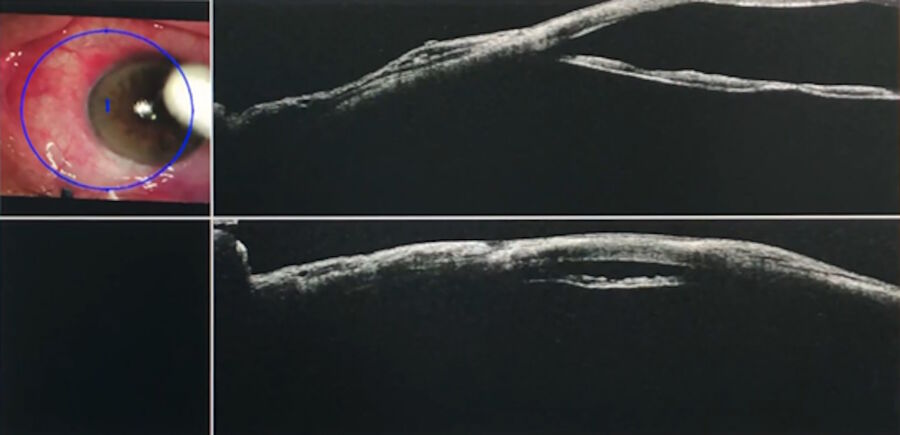
A 73-year-old male patient with chronic primary open-angle glaucoma had had a glaucoma surgery (trabeculectomy) three weeks before. Unfortunately, the intraocular pressure (IOP) was not as low as expected. The anterior segment examination revealed an encapsulated bleb which needed to be addressed.
The operation took place under topical anaesthesia. Standard needling was performed with a bent 25-gauge needle to enter under the scleral flap and conjunctiva. The EnFocus Intraoperative OCT was used to visualize the two different planes, offering greater control than visualization through the microscope only. It showed the bleb no longer had cystic walls.
A local massage was also performed during the procedure. At the end of the intervention, and after needling, intraoperative Optical Coherence Tomography was used to check the filtration flow through the bleb. It confirmed that there was good drainage under the scleral flap.
Glaucoma surgery clinical case 2: Needling of post-trabeculectomy failed flat bleb
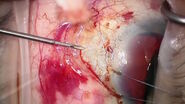
In this clinical case, a 64-year-old male patient with advanced primary open-angle glaucoma also underwent trabeculectomy. After the operation, his intraocular pressure was not satisfactory, and the anterior segment examination showed a flat bleb. Two weeks after the first procedure, he was reoperated to needle the flat bleb.
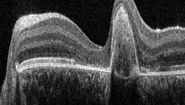
The EnFocus intraoperative OCT was useful to see the three surgical planes. The surgeon first entered with a bent needle under the scleral flap, between the scleral flap and the scleral bed. Afterwards, she entered between the scleral flap and conjunctiva or tenon, which was fibrotic.
The images showed clearly the two different spaces between the three planes: the scleral flap, the scleral bed and the conjunctiva and tenon. Intraoperative OCT helped visualize these spaces created by surgical manoeuvres. In addition, through massage, it was possible to observe the good drainage after needling of the flat bleb.
As such, intraoperative OCT is a useful tool to support glaucoma surgery procedures. It allows to visualize the surgical planes and verify drainage.
Please note that off-label uses of products may be discussed. Please check with regulatory affairs for cleared indications for use in your region. The statements of the healthcare professionals included in this clinical case reflect only their opinion and personal experience and not those of Leica Microsystems. They also do not necessarily reflect the opinion of any institution with whom they are affiliated.